Skin cancer is the most common form of cancer in the United States, with approximately 9,500 people diagnosed per day, and melanoma rates having doubled between 1982 and 2011. Melanoma is the deadliest form of skin cancer.
Exposure to UV light is the most preventable risk factor for all skin cancers, and if you spend a lot of time in the sun, either for work or pleasure, your risk of getting skin cancer is already high. Risks increase if you have fair skin and hair, blue or green eyes, freckles or regularly use artificial sun beds and UV lamps.
Prevention is essential to avoid this potentially fatal form of cancer, while early detection greatly improves prognosis and treatment outcomes.
Prevention
The most effective way of protecting your skin from the sun is to cover it with clothing and sunscreen. The sun is usually strongest between 11 a.m. and 3 p.m. so it’s best to avoid direct sunlight during these hours.
If you can’t, apply a water-resistant sunscreen with a high UVA rating and an SPF of at least 30 every two hours (more frequently if you are swimming or exercising), and never use a sunscreen that has gone beyond its expiry date. Protect your eyes and scalp with sunglasses and a wide-brimmed hat.
Self-examination
The American Academy of Dermatology and The Skin Cancer Foundation encourage everyone to perform regular skin self-exams to check for signs of skin cancer as about half of melanomas are self-detected.
“Ideally you should examine your skin once a month,” says adult and pediatric dermatologist Dr. Alison Duncan of TrinCay Medical Services Ltd. “Look everywhere for a new or changing mole and slowly growing patches or lumps which do not heal.”
Using a bright light, full length mirror, hand mirror, two chairs, and a hair dryer where necessary, examine every part of your body for lesions and make a note of them on a body map.
Examine your entire body — front and back — using a full-length mirror. Then, look at your right and left sides with your arms raised.
Bend your elbows and look carefully at your forearms, underarms and palms.
Look at the backs of your legs and feet, the spaces between your toes, and the soles of your feet. Check your fingernails and toenails, with nail polish.
Examine the back of your neck and scalp with a hand mirror. Part your hair for a closer look.
Finally, check your back and buttocks with a hand mirror. Consider asking a partner to help, as another set of eyes can be helpful for checking the back and other hard-to-see areas.
ABCDEs
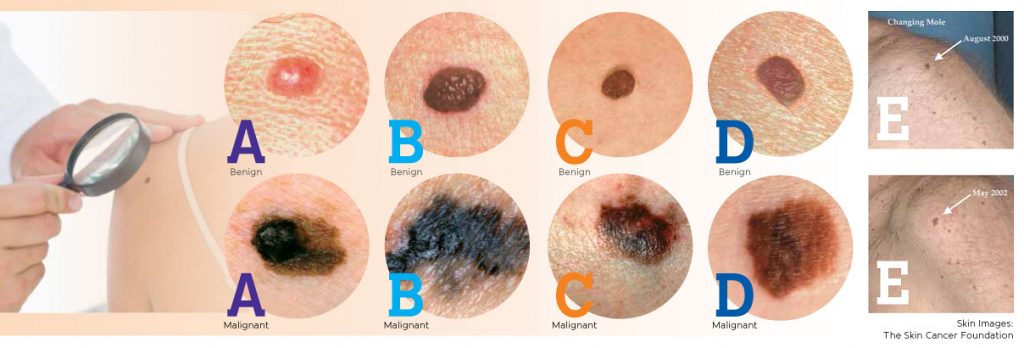
Two specific strategies have been developed for early recognition of melanoma,: the ABCDEs and the Ugly Duckling sign (recognizing a mole that stands out at first glance).
If you see one or more of the ABCDE signs of melanoma, make an appointment with a physician immediately.
Click to enlarge
A – Asymmetry
This benign mole is not asymmetrical. If you draw a line through the middle, the two sides will match, meaning it is symmetrical. If you draw a line through this mole, the two halves will not match, meaning it is asymmetrical, a warning sign for melanoma.
Images:
A – Benign – Caption: Benign
A – Malignant – Caption: Malignant
B – Border
A benign mole has smooth, even borders, unlike melanomas. The borders of an early melanoma tend to be uneven. The edges may be scalloped or notched.
Images:
B – Benign – Caption: Benign
B – Malignant – Caption: Malignant
C – Color
Most benign moles are all one color — often a single shade of brown. Having a variety of colors is another warning signal. A number of different shades of brown, tan or black could appear. A melanoma may also become red, white or blue.
Images:
C – Benign – Caption: Benign
C – Malignant – Caption: Malignant
D – Diameter
Benign moles usually have a smaller diameter than malignant ones. Melanomas usually are larger in diameter than the eraser on your pencil tip (¼ inch or 6mm), but they may sometimes be smaller when first detected.
Images:
D – Benign – Caption: Benign
D – Malignant – Caption: Malignant
E – Evolving
Common, benign moles look the same over time. Be on the alert when a mole starts to evolve or change in any way. When a mole is evolving, see a doctor. Any change — in size, shape, color, elevation, or another trait, or any new symptom such as bleeding, itching or crusting — points to danger.
Image:
Evolve – No Caption
Source: The Skin Cancer Foundation. For more information, visit www.SkinCancer.org
Images: The Skin Cancer Foundation
Mole mapping
Mole mapping is another term for photographic skin surveillance which is an advanced method for monitoring moles which is painless and noninvasive.
“This involves whole body clinical examination and dermoscopy, total body photographs and close up dermoscopic photographs of moles and skin lesions,” explains Dr. Duncan. “These images are then used to detect new lesions or changing lesions to aid in the monitoring and early detection of skin cancer.”
The method is useful for anyone who has multiple moles or a history of abnormal moles; moles which are difficult to self-monitor such as those on the back; a previous history of melanoma; fair skin that has been severely or repeatedly sunburned; or a changing or enlarging mole.
If something untoward is shown by mole mapping, there are a few possible next steps.
“Overtly abnormal moles will be removed in a timely fashion for assessment under the microscope for melanoma at the first review,” says Dr. Duncan, who also notes that photographic surveillance can be used to monitor moles at three-month, six-month or yearly interval for change.
“If a change is noted to the size, structure or the color of the mole then it is suspicious for melanoma,” she continues. “The mole can then be excised (cut out) using local anesthetic and assessed at a microscopic level for cells which are indicative of melanoma.”
Not all dermatologists offer mole mapping so check with your healthcare provider for their full remit of services.
Cayman Dermatologists
Dr. Else Christoffersen – Cayman Doctors Ltd., West Shore Center 943-6363
Dr. Andrea Clare-Lyn Shue – Health Services Authority, Cayman Islands Hospital 949-8600
Dr. Rebeca De Miguel – Celimar Central Clinic, Governors Square 925-2512
Dr. Alison Duncan – Trincay Medical Services Ltd, Camana Bay 943-4633
Dr. Julia Kirschke – NovoClinic, Eastern Avenue 746-6082
Dr. Wayne Porter – Dr. Wayne Porter’s Practice, Crewe Rd. 946-9020